If you think your MS may be changing, it’s time to start pushing back
Consultations can be short—reflect on any changes in your MS over the past 6 months to have a more focused and optimized conversation with your healthcare team.
The MS Journey
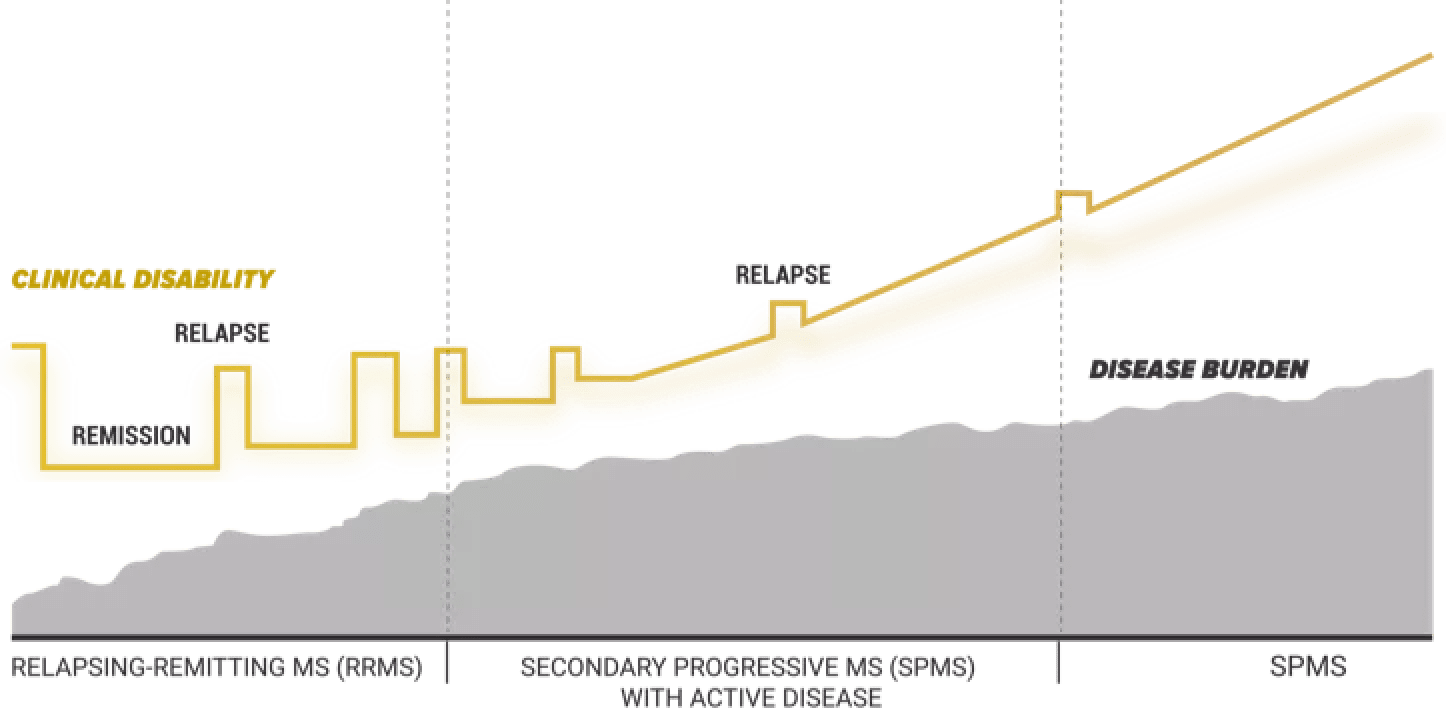
Multiple sclerosis (MS) doesn’t look the same for everyone. When people think of MS, they commonly think of relapsing-remitting MS (RRMS). But secondary progressive MS (SPMS) is a different phase that not many people are talking about.
Understanding MS starts with the basics
There is more than 1 phase with MS. But they are all at different stages of progression.
Frequency of relapses matter
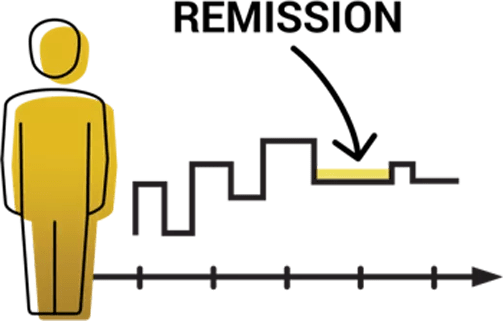
To be labeled a new relapse, there must be 30 days of stability (remission) in between cognitive or physical symptoms. If your MS begins changing, however, you may or may not bounce back from a relapse as well as before, or your symptoms may not go away completely. This may get in the way of doing everyday activities. While everyone is different, studies show that more frequent relapses early on may lead to a higher likelihood of progression down the road.
RRMS may progress to SPMS
Most people with RRMS eventually develop a different kind of MS called SPMS. This happens gradually over many years, causing symptoms to get worse overall. This can potentially lead to more noticeable symptoms or increased disability.
Identifying MS progression
Frequency of relapses matters
The progression of MS can be hard to detect. Your symptoms may become more challenging and you may even experience fewer relapses. Symptom-tracking tools like the Your MS Questionnaire can help you identify any changes in your MS over a period of time, empowering you to have more focused discussions with your healthcare team. The sooner you tell your doctor about your MS changes, the better the chance you may have of delaying progression.
How to tell if your MS is changing
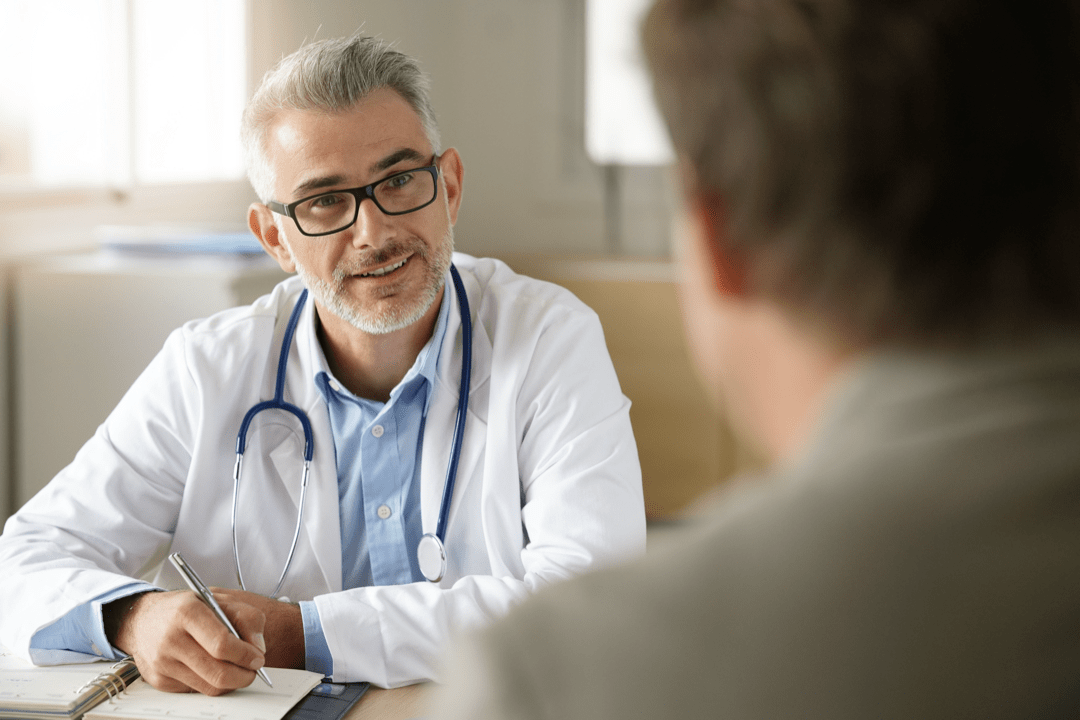
To determine if your MS is progressing, your doctor needs to know two important things: how long you’ve had MS, and how your MS has changed over time. Here are some signs you should look out for:

Your symptoms are getting worse, you’re experiencing new ones, or they’re lingering between relapses

Mental activities are harder than they were in the past.
Physical activities are harder to do than they were in the past.

Relapses may occur less often.
Common signs of your MS changing to SPMS
Cognitive Changes

Difficulty finding words or trouble speaking

Worsening memory

Trouble thinking quickly and clearly
Physical Changes

Difficulty with movement, balance, and walking

Bladder and bowel problems
Fatigue and feeling extremely tired
What’s going on inside your body
There are 2 things in common with all stages of MS progression: the central nervous system (CNS) and inflammation.

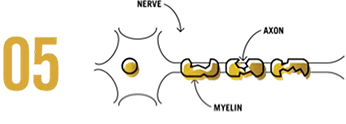
MS affects your CNS, which includes your brain and spinal cord. It's made up of nerves that send signals all around your body. These signals control many things, such as balance, coordination, and memory.
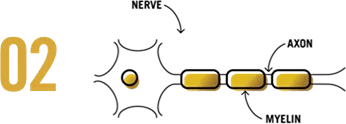
White blood cells in your immune system mistake the coating around your nerves (myelin) and nerve fibers (axons) for something that shouldn't be there. Think of myelin as the insulation around electric cables.

The white blood cells then attack the myelin, creating inflammation, which damages the myelin and exposes the axons
When myelin is damaged, signaling slows or becomes disrupted, which may cause relapses. A relapse can last anywhere from a day to months, until the brain can repair the damage.
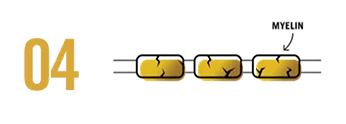
As MS damages your nerves over time, there may be little or no myelin left.
Therefore, there is nothing to become inflamed or cause a relapse.
You may also start to see lesions appearing or becoming bigger on MRI scans
Disability starts to build up over time
Damage to your nerves (neurodegeneration) builds up, which causes symptoms to worsen This can lead to disability that can impact your daily activities.
Talking to your doctor
How were you feeling a few months ago
Think back to how you were feeling 6 to 12 months ago. Then consider whether you’ve noticed any changes since then, like your ability to accomplish mental and physical tasks. If your symptoms have changed over the past 6 months, it’s important to let your healthcare team know.
Speaking up about symptom changes
Signs and symptoms of MS are different for everyone. If you feel that your MS is changing, it’s important to be proactive. By sharing symptoms as soon as they appear, you and your healthcare team can have an informed discussion about any changes in your MS.
Below is a chart to help you decide when it's important to discuss your changing MS with your doctor.

The white blood cells then attack the myelin, creating inflammation, which damages the myelin and exposes the axons

Does the symptom persist?
YES: Schedule follow-up appointment
NO: Keep watch for symptom change

Does the symptom persist?
YES: Discuss persistent symptom changes with your healthcare team
NO: Keep watch for symptom changes

Preparing for your next consultation
The Your MS Questionnaire asks about your MS in the past 6 months including any relapses, your symptoms, and their impact on your daily life. This information will empower you to have a focused discussion with your healthcare team about any changes to your MS. You may wish to ask a family member, partner, or caregiver for help when completing the questionnaire.
Caregiver contributions matters
When a loved one’s MS is changing, things may become different than they were before—but the more you know, the more you can help them during this transition. It may be difficult for people with MS to notice their symptoms changing or worsening. That's why it's important to support your loved one by being honest about any changes you may have noticed. Your input can help make a difference in the management of your loved one's MS. Don’t hesitate to ask questions every step of the way. You, your loved one, and their healthcare team can come up with a plan to help navigate your loved one's MS journey


Be mindful of changes
Your perspective on how your loved one is doing matters. It’s important to notice how their MS changes over time, and to help them have an honest conversation with their healthcare team.
You can also assist your loved one in completing the Your MS Questionnaire. Your perspective on their MS can lead to more informed conversations with their healthcare team.
The SPMS Conversation Starter can help make the discussion easier.
You can use it to:
- Record how MS is affecting your loved one now, compared with 6 to 12 months ago
- React to what you have observed
- Use those observations to spark a conversation with your loved one’s healthcare team


Sharing a language
RRMS. SPMS. Progression. There is a new vocabulary your doctor may be using to describe the changes with your loved one. Understanding these terms can help make conversations with your loved one and his or her medical team more effective.
Here are some terms that might be helpful in understanding SPMS:
- Relapses: A period of time when your loved one’s symptoms suddenly worsen
- RRMS: The phase of MS your loved had before SPMS, relapsing-remitting MS (RRMS) is characterized by periods of relapse and partial recovery.
- SPMS: This phase of MS comes after a person has had RRMS for many years. Your loved one may have fewer relapses, but new or worsening symptoms may accumulate.
- MS progression: As MS progresses, your loved one may experience new or worsening symptoms, and increasingly struggle with daily activities and chores.
- Neurodegeneration: Damage to the nervous system -particularly the brain- that is the cause of your loved one’s symptoms.